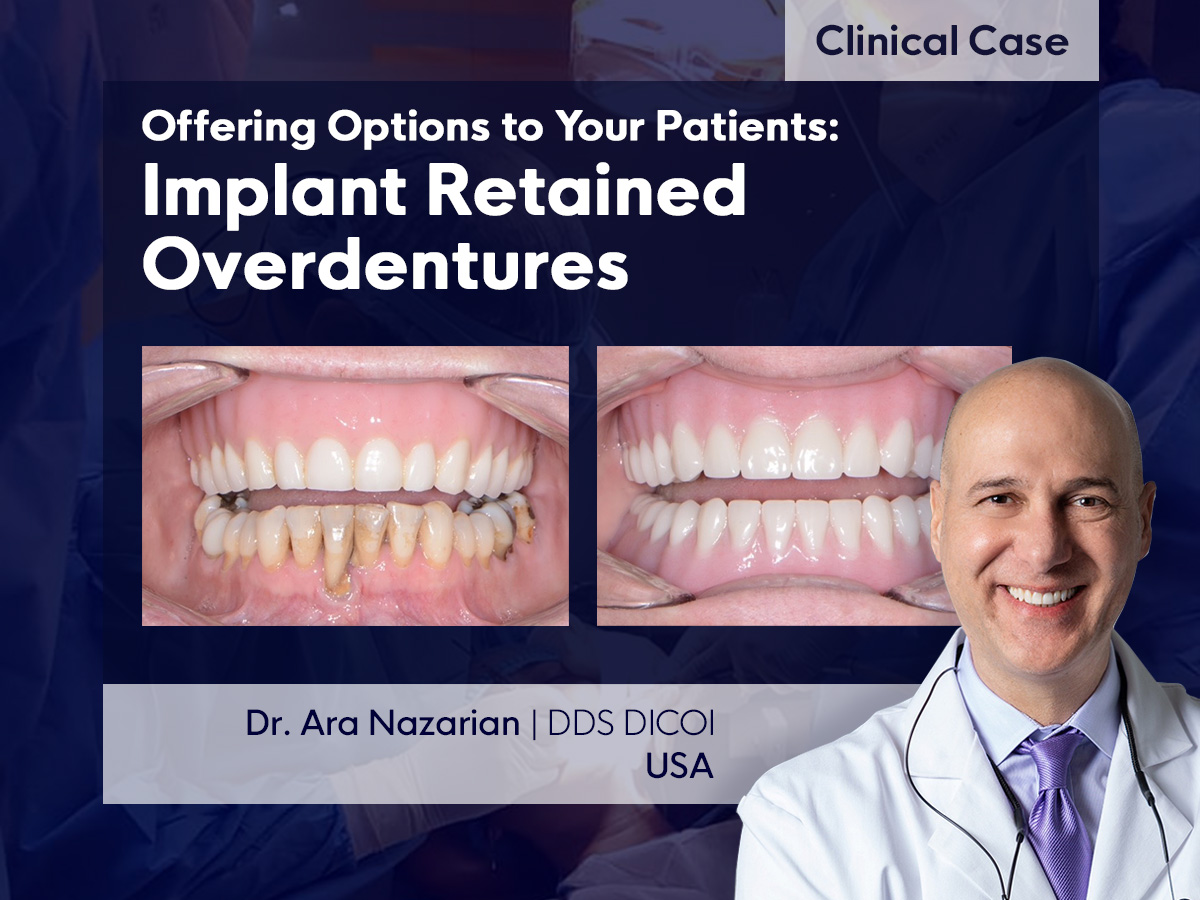
A 59-year-old male patient who has been utterly edentulous for more than thirty years came to our office expressing great dissatisfaction with the stability of his prosthesis and apprehension about dental procedures.
The examination shows an upper total prosthesis with significant levels of wear and a lower arch restored with a lower partial prosthesis and teeth with periodontal involvement.
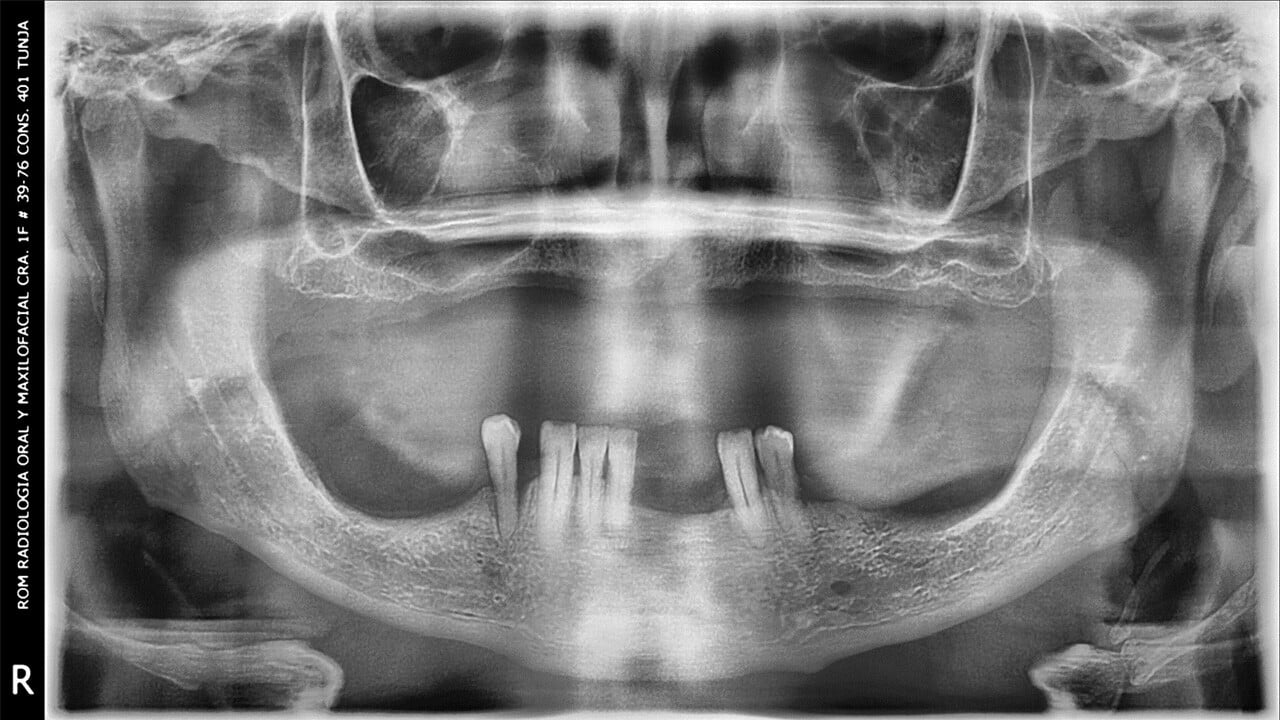
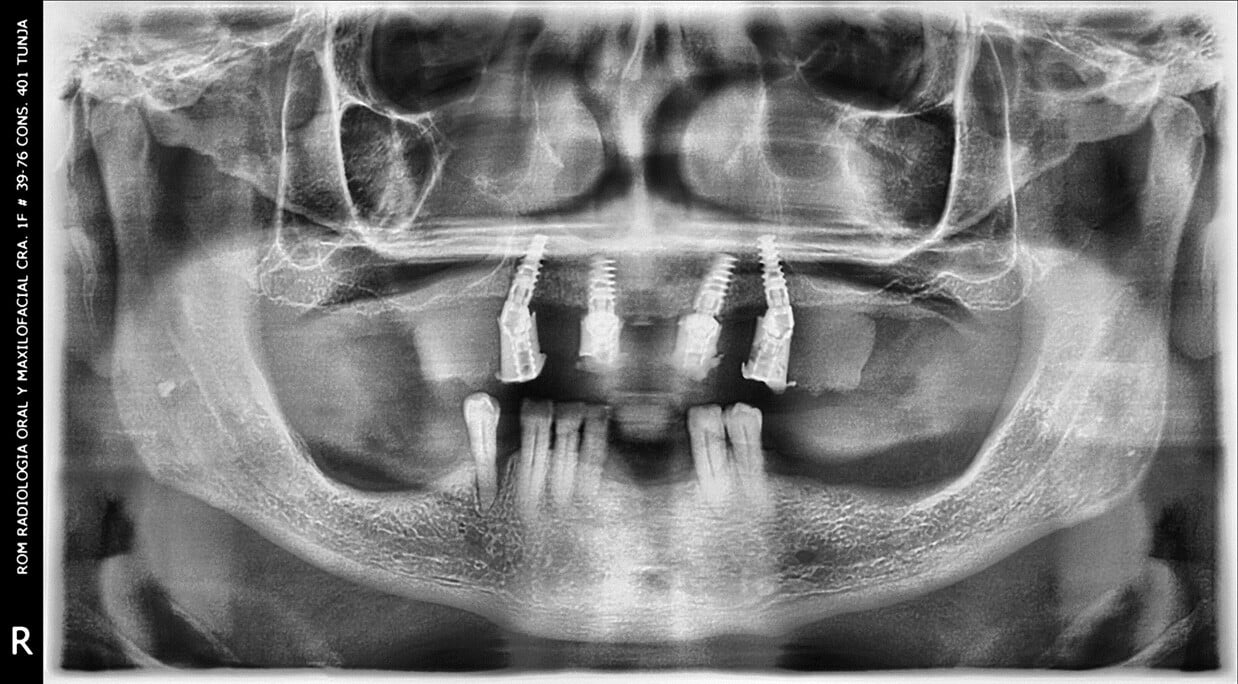
Pre-operative x-ray
Intraoral Conditions
- Upper total edentulous with poorly adapted prostheses.
- Lower partial edentulous with poorly adapted prostheses and remaining teeth affected by periodontal disease.
- Bilateral maxillary sinus pneumatization, which limits the placement of implants in the posterior sector.
- Very limited bone ridge in the maxillary anterior zone in height and width.
Proposed Treatment Plans
The different prosthetic alternatives are discussed within the following options
1. Conventional upper total prosthesis Vs. partial extraction and lower removable prosthesis, with limitations on stability and retention.
2. Fixed implant-supported prosthesis with bilateral sinus lift Vs. fixed implant-supported inferior prosthesis (All on X technique).
3. Fixed implant-supported superior prosthesis with stackable guide protocol and placement of the posterior implants in an angled position to avoid maxillary sinus and immediate temporary prosthesis restoration designed by computer.
Patient Decision
After discussing the different options, the patient, considering his need to perform the fewest surgical interventions and that they would take a not very long time, decides to perform only the restoration of the upper arch initially, without grafts, additional surgical time, and under a guided protocol, with the possibility of leaving the surgical procedure with the temporary fixed prosthesis.
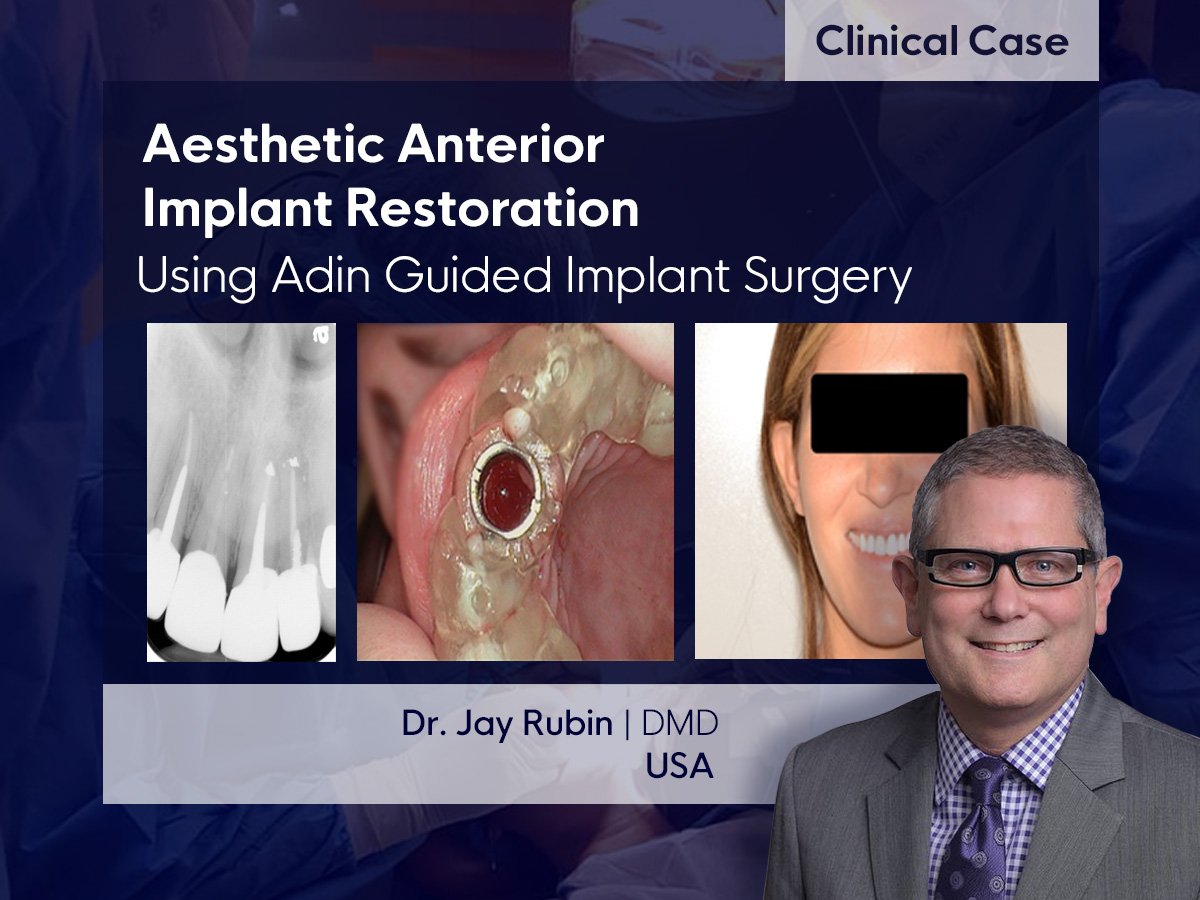
Digital Planning
Initial records were made for digital planning:
- Double CBCT technique (patient with prosthesis and prosthesis)
- Clinical photos
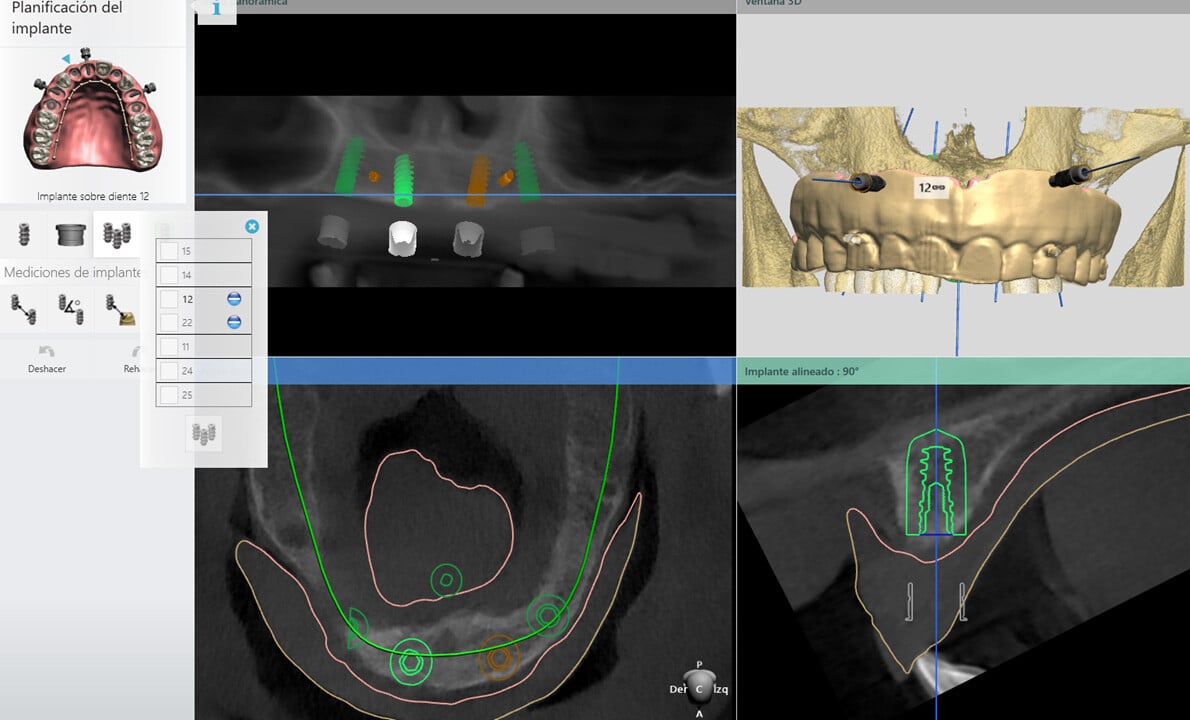
The double scan allows us to see the patient's occlusion and the distribution of teeth in the mouth to plan the placement of the implants digitally. We know in advance the angulation of the implants to avoid the area of the maxillary sinus, optimize the anteroposterior distribution, and improve the load on the implant-supported fixed prosthesis.
Digital planning also allows us to plan the height and angulation of the multiunit TMA (Trans Mucosal Abutments), optimizing the prosthetic resource.
The planning software also allows us to know bone density and the implications for surgical execution.
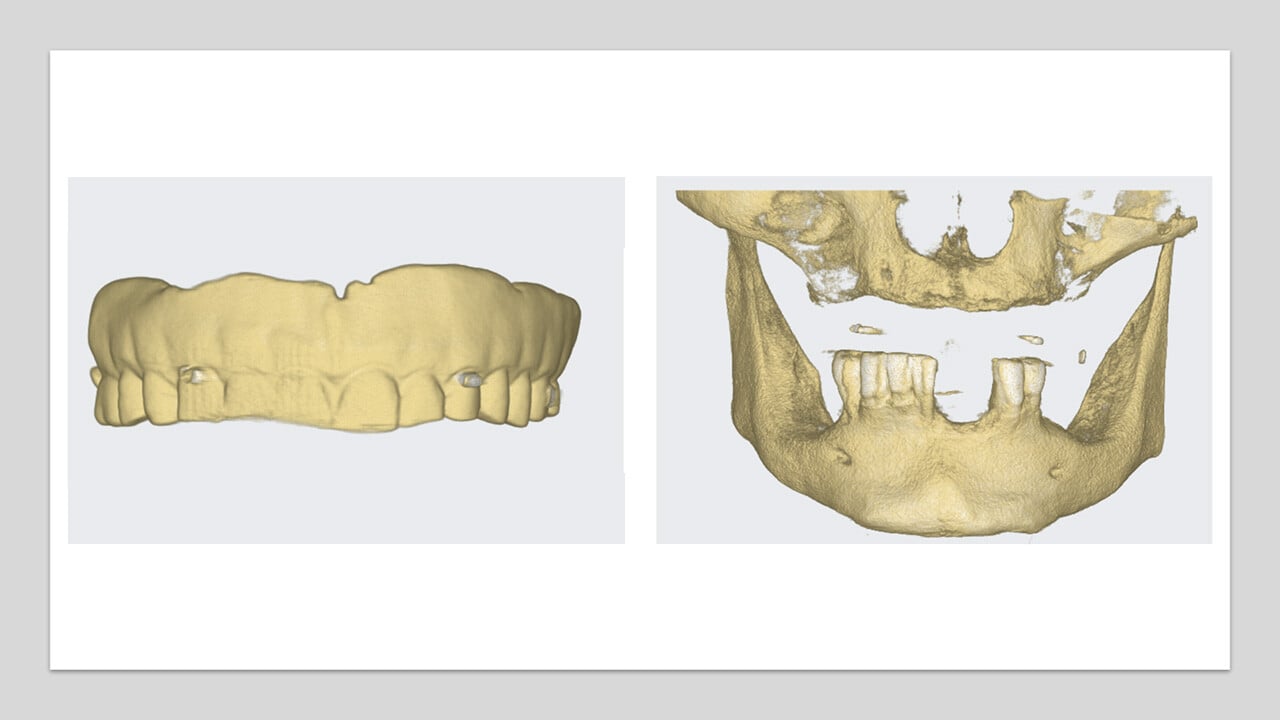
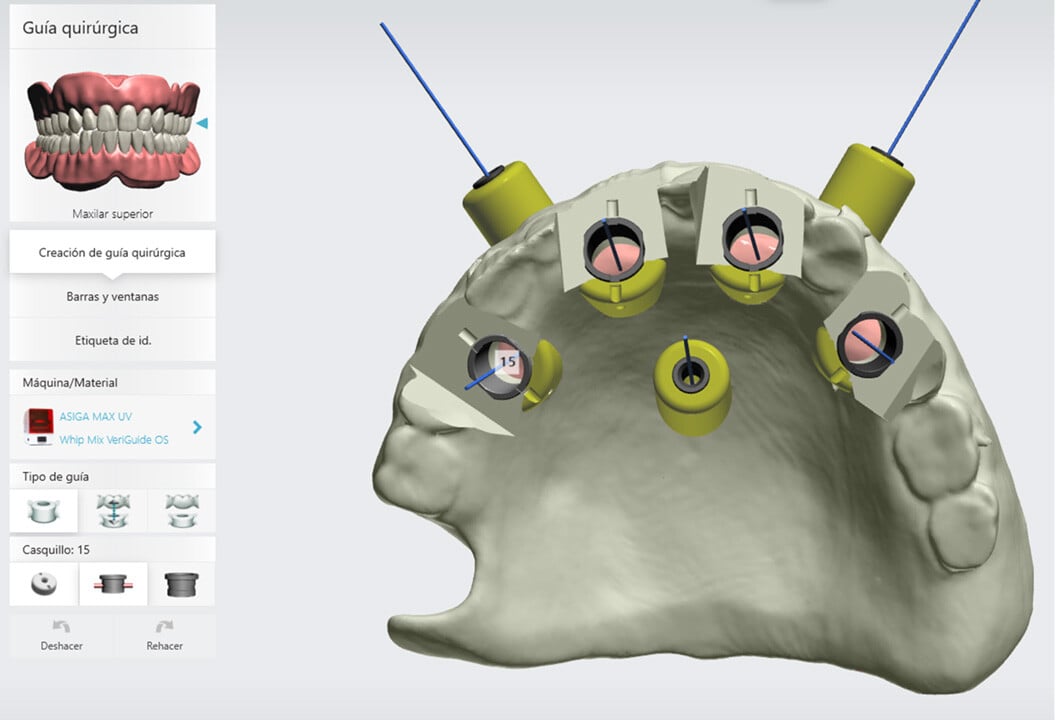
The patient's prosthesis was used as the basis for the surgical guide, converting it to STL.
It was decided to place Touareg-OS implants of Adin due to their high primary stability in low-density bone substrates; their conical design with self-tapping capacity is ideal for these types of bone.
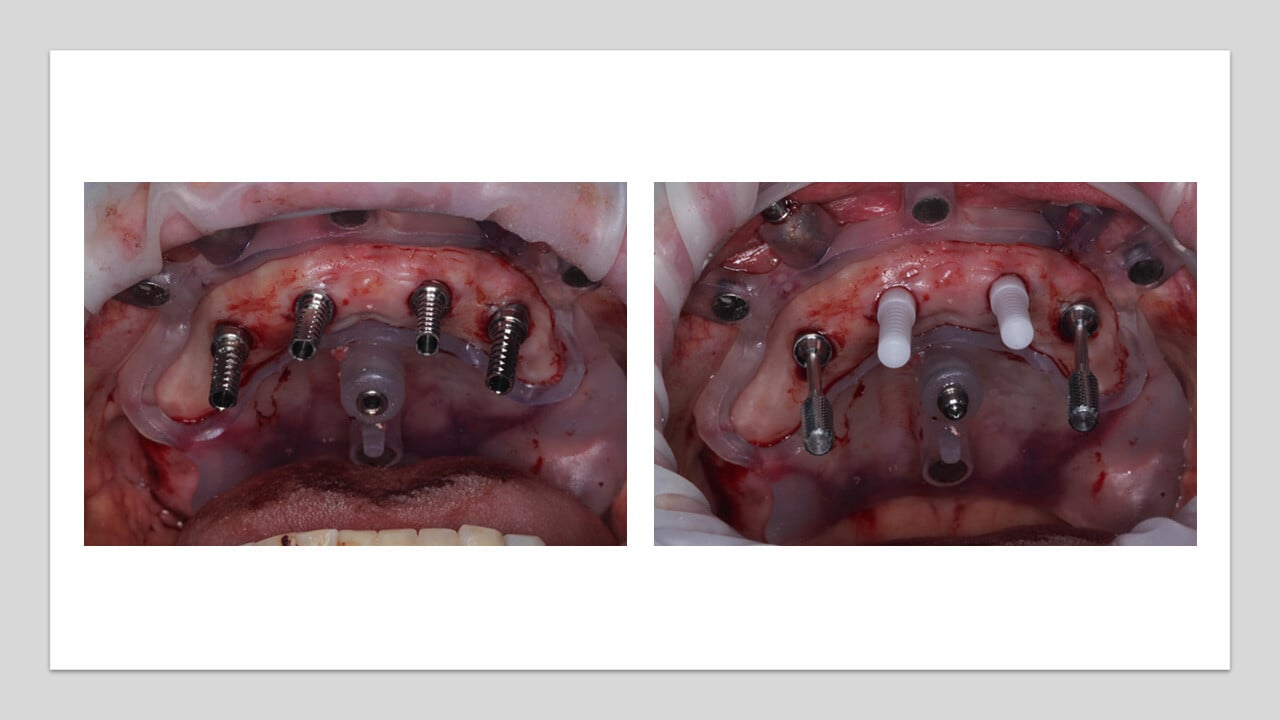
Adin's guided surgery protocol allows us to accurately place 100% parallel implants (diameter 10 x 3.75) in zones 12 and 22 and angled at 17 degrees in zones 14 and 24 (11.5 x 3.75).
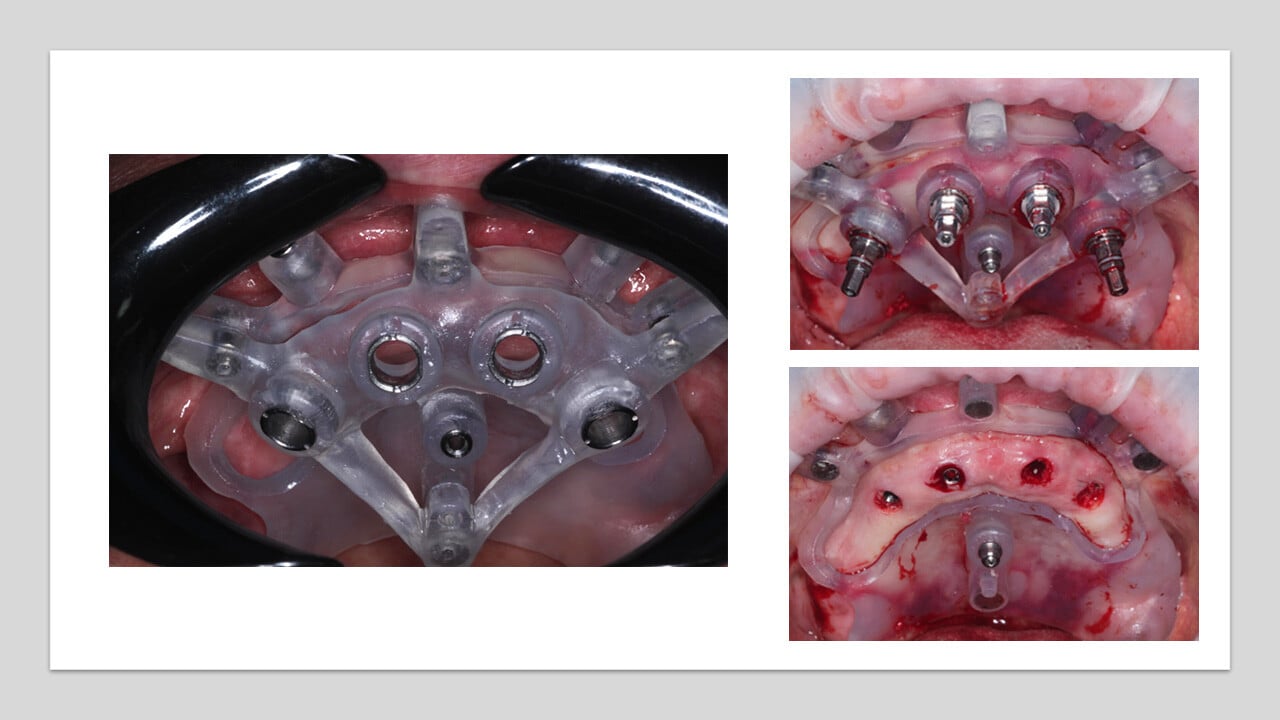
Three fixation screws were placed for the guide in tripoidal distribution to increase the stability of the mucosa-supported guide.
Implants should be Mountless for Adin's guided surgery protocol, which allows us to install an immediate temporary prosthesis elaborated in PMMA in a very short intraoperative time. This reduces the operator's chair time and clinical stress, with high predictability in occlusion and minimal adjustments in the postoperative period.

Implementation
Under flapless surgery protocol and stackable guides, 4 implants were placed in the upper maxilla with the planned distribution and angulation using a guide from the modified copy of the patient's current prosthesis, anchored with fixation screws.
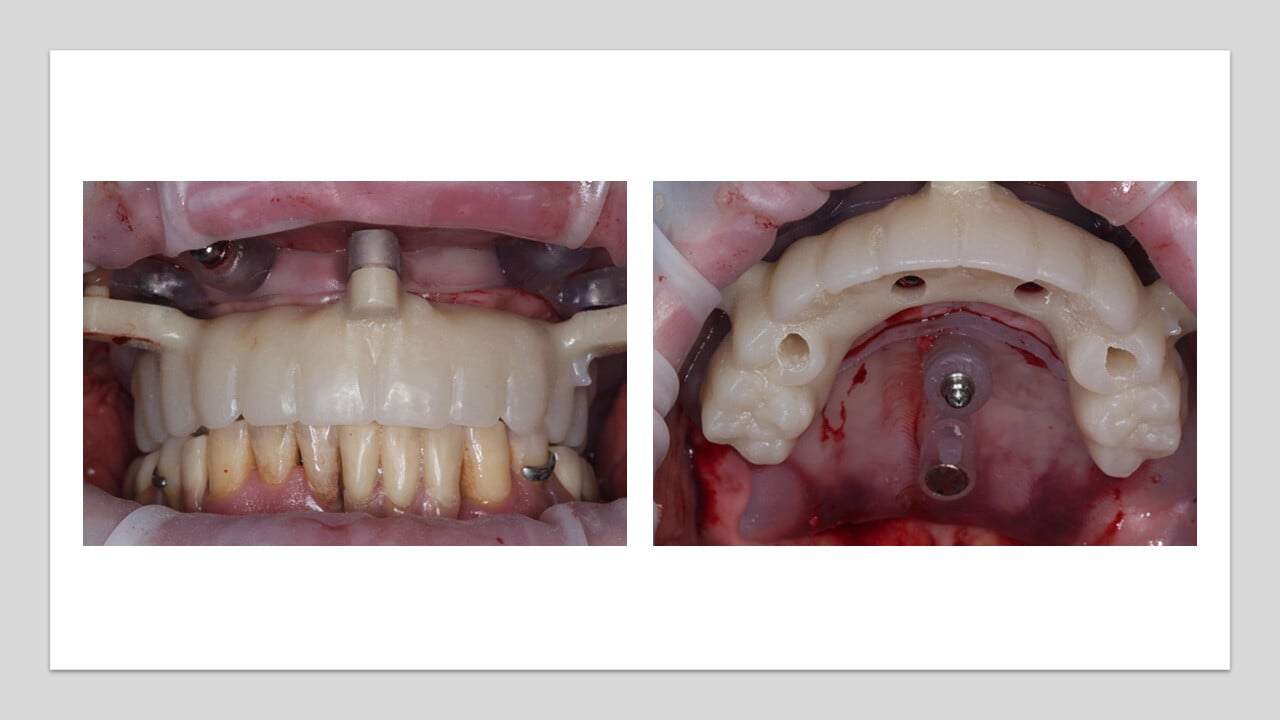
We placed four Multinuit Transmucosal Abutments of Adin: two straights in positions 12 and 22 and two angled at 17 degrees in 14 and 24.
Four metallic temporary Abutments were placed, and then a PMMA immediate prosthesis was fixed based on the stackable guide. A high-precision coincidence of the occlusion between planning and execution was verified.
The procedure had a total execution time with restoration of only two hours.


Conclusions
Stealable guided protocols with adin are very predictable and allow us to obtain optimal primary stability for immediate restoration.
This case allowed us to solve, using a fixed prosthesis supported by implants, the requirements of a patient with anxiety in the face of lengthy and invasive surgical procedures.
The use of Adin-guided implants facilitates agile and predictable surgical execution with an immediate restoration that saves surgical times and reduces intraoperative and postoperative complications.
The predictability of guided procedures is based on an adequate imaging protocol, data processing, and efficient execution.